Services
Call Us
Hours
Monday: 8 AM – 4:30 PM
Tuesday: 8 AM – 4:30 PM
Wednesday: 8 AM – 4:30 PM
Thursday: 8 AM – 4:30 PM
Friday: 8 AM – 2:30 PM
Download

About Florida Eye Surgeons And Associates
At Florida Eye Surgeons and Associates, our multi-specialty ophthalmic practice is committed to providing outstanding medical and surgical eye care, strongly emphasizing advanced retinal treatment. With skilled physicians trained extensively in retinal procedures, we’re equipped to address a wide range of eye care needs. Our retinal services span cutting-edge treatment for macular degeneration, retinal retinopathy, retinal vascular diseases, and retinal detachments. Backed by our reputation and positive patient experiences, you can trust us for personalized and compassionate eye care that prioritizes your vision and well-being.
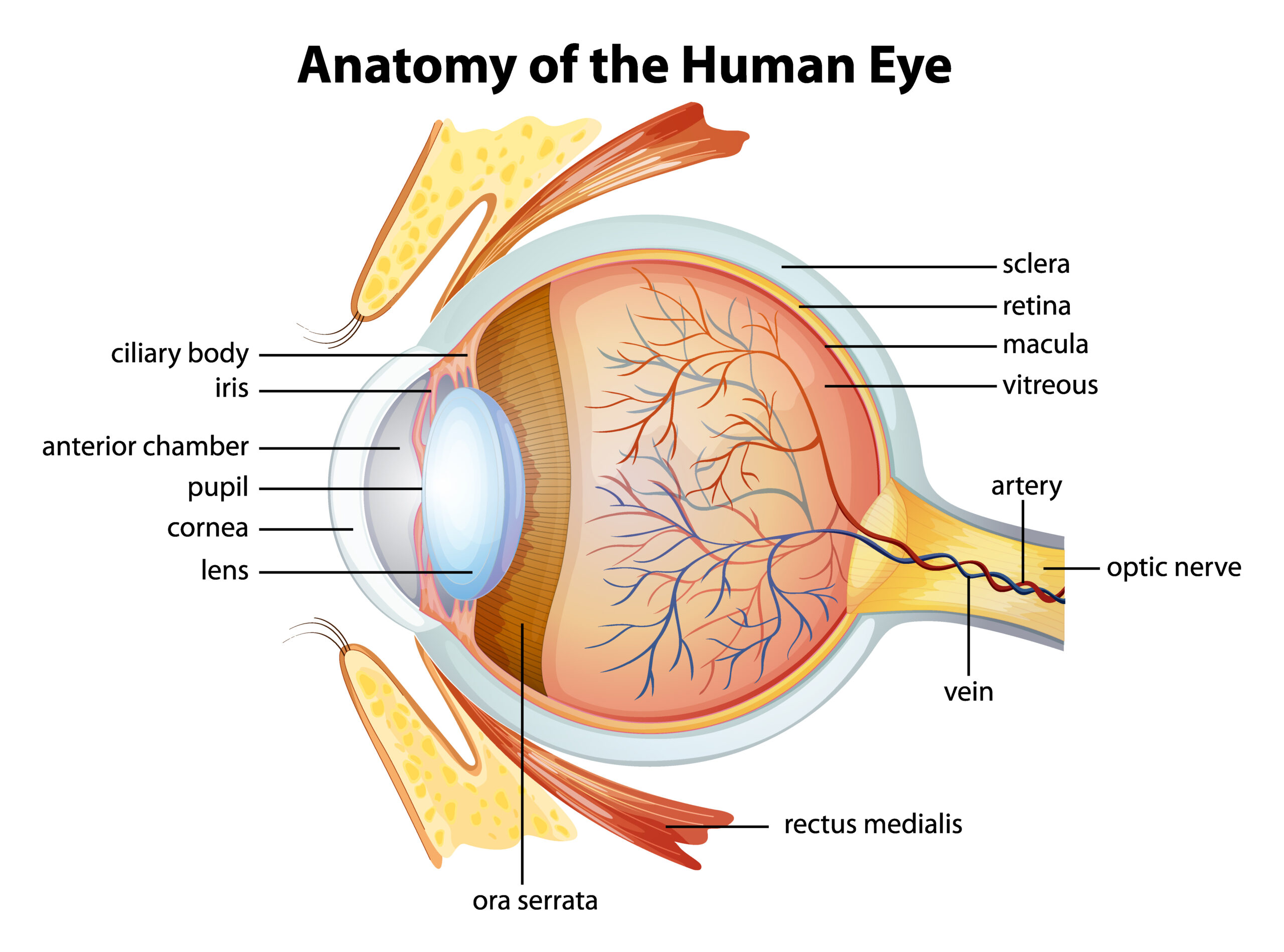
What Is The Retina?
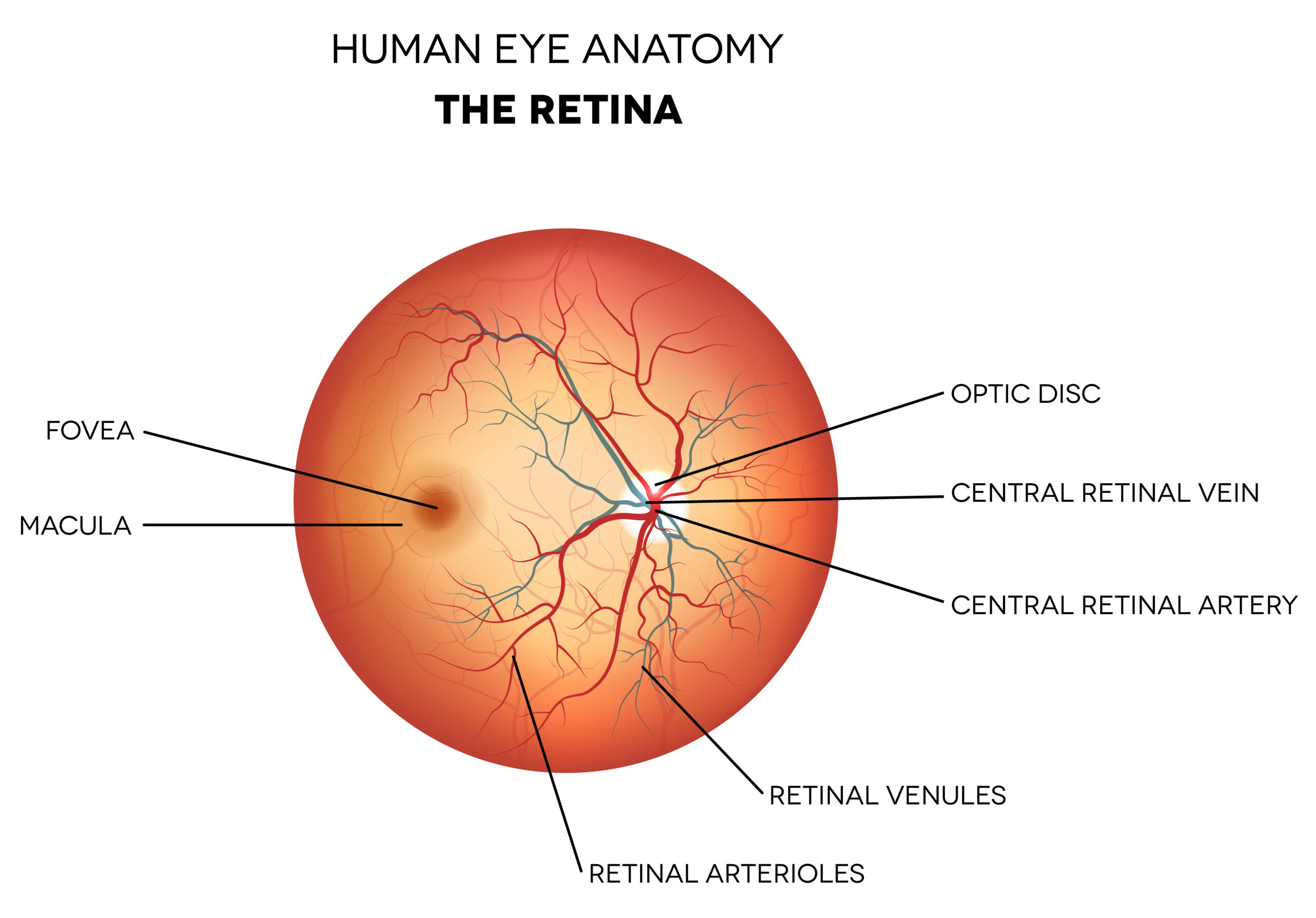
The retina is a thin layer of tissue at the back of the eye. It plays a crucial role in vision by capturing light that enters the eye and converting it into electrical signals. These signals are then sent through the optic nerve to the brain, where they are interpreted, allowing us to see the world around us.
Various eye conditions and diseases can affect the retina, leading to vision problems or vision loss. Regular eye exams are essential for detecting retinal issues early and ensuring timely intervention and treatment.
What Are Common Medical Conditions That Affect The Retina?
Various medical conditions affect the retina, and while not all may require retina surgery, many of these conditions can be effectively treated with surgical interventions. Our skilled retinal surgeons are experienced in providing tailored treatment options to address retinal diseases to preserve or improve your vision.
Macular Degeneration is an age-related eye condition that causes progressive damage to the macula (the anatomical area of the retina that is responsible for detailed vision), resulting in central vision loss. Treatment options for macular degeneration include medications, laser therapy, and in some cases, injections to slow down its progression and preserve remaining vision.
Diabetic Eye Disease is a complication of diabetes that can affect the retina, leading to vision problems and potential blindness. Treatment for diabetic eye disease may include laser therapy, injections, or surgical interventions to prevent further vision loss.
Flashes and Floaters are common symptoms that may indicate a posterior vitreous detachment or other issues within the eye. Eye floaters are small, often transparent, spots or squiggles that seem to float in your field of vision. While most cases do not require treatment, it is essential to have a comprehensive eye examination to rule out any severe underlying conditions and receive appropriate care.
A Detached Retina is a serious eye condition where the retina separates from the inner wall, potentially causing severe loss of vision. Treatment options for retinal detachment include surgical procedures to reattach the retina and prevent permanent vision impairment.
Who Is At Risk For Developing Retinal Conditions?
Several factors can increase your risk of developing retinal issues. Individuals at higher risk include those with these conditions:
- Advanced Age: Retinal conditions, such as age-related macular degeneration (AMD), are more common as people age, particularly in individuals over 60.
- Family History: A family history of retinal disorders, such as retinal detachment or hereditary retinal diseases, can elevate the risk.
- Diabetes: Diabetic eye disease is a significant risk factor for retinal issues, particularly if diabetes is poorly controlled.
- High Blood Pressure: Hypertension (high blood pressure) can increase the risk of retinal vascular diseases and retinopathy.
- Smoking: Smoking has been linked to an increased risk of developing retinal conditions, including AMD.
- High Myopia (Nearsightedness): Individuals with high myopia may be at a higher risk of retinal issues such as retinal detachment or myopic macular degeneration.
- Previous Eye Trauma or Surgery: A history of eye injuries or eye surgeries may elevate the risk of retinal problems.
- Inflammatory Diseases: Certain inflammatory conditions or autoimmune diseases can increase the risk of developing retinal issues. It’s essential to note that even individuals without these risk factors can still develop retinal issues, and regular eye exams are crucial for early detection and timely management. If you have any concerns about your eye health or are at risk for retinal conditions, consult our eye care professionals for a comprehensive evaluation and appropriate care.
Why Choose Florida Eye Surgeons And Associates?
Florida Eye Surgeons and Associates takes pride in our educated team of medical professionals who use advanced technology to focus on your eye health. Our commitment to individualized care and the highest level of service make our practice different. When you come to us, you can rest assured that your eyes are in the best hands.
Contact us for all of your eye care needs. We look forward to helping you work toward a brighter future.
